Rectal Prolapse: Symptoms, Causes & Treatment
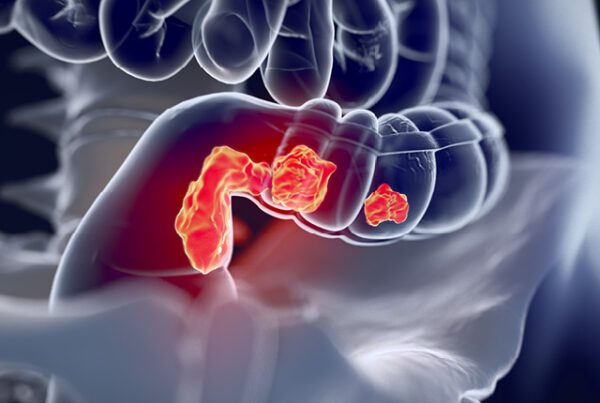
Rectal prolapse is a condition where the rectum, which is the lower part of the colon or large intestine, protrudes or falls out of the anus. It can range from a partial prolapse, where only the lining of the rectum protrudes, to a complete prolapse, where the entire rectum extends through the anus. This condition can be uncomfortable, and embarrassing, and affect daily activities.
Rectal Prolapse Causes and Risk Factors:
- Weak Muscles and Ligaments: Weakening of the muscles and ligaments that support the rectum, often due to aging, childbirth, chronic constipation, or repetitive straining during bowel movements.
- Chronic Straining: Conditions that cause chronic straining during bowel movements, such as constipation or long-term diarrhea, can increase the risk of rectal prolapse.
- Previous Surgery or Injury: Previous pelvic or rectal surgery, injury, or conditions that affect the pelvic area can weaken the rectal support structures.
- Neurological Conditions: Certain neurological conditions like spinal cord injury or multiple sclerosis can affect the nerves that control the rectal muscles, contributing to prolapse.
- Protrusion: Visible protrusion of the rectum through the anus during or after bowel movements.
- Bowel Movements: Difficulty with bowel movements or a feeling of incomplete evacuation.
- Anal Leakage: Incontinence or leakage of stool or mucus.
- Bleeding: Blood or mucus in stools or on toilet tissue.
- Discomfort or Pain: Discomfort, pain, or a sensation of fullness in the rectal area.
Treatment Options:
The Treatment of Rectal Prolapse depends on the severity of the condition and the individual’s overall health. Here are some common approaches:
- Conservative Management:
- Dietary Changes: Increasing fiber intake to prevent constipation and reduce straining during bowel movements.
- Pelvic Floor Exercises: Performing pelvic floor muscle exercises (Kegel exercises) to strengthen the pelvic floor muscles.
- Lifestyle Modifications: Avoiding heavy lifting and activities that strain the pelvic area.
- Medical Management:
- Medications: In some cases, medications such as stool softeners or laxatives may be prescribed to relieve constipation and ease bowel movements.
- Surgery: Open and Laparoscopic
- Rectal Prolapse Repair (Rectopexy): Surgical repair is often the most effective treatment for rectal prolapse. The specific technique used will depend on the extent and type of prolapse. Procedures may involve repositioning, fixing the rectum to its normal position, and reinforcing the supporting structures.
- Perineal Approach: Some procedures can be performed through the perineum (the area between the anus and the external genitalia), avoiding an abdominal incision.
- Abdominal Approach: Other surgeries may require an abdominal approach, involving a laparoscopic or open surgery.
- Bowel Resection: In severe cases where the rectum is extensively damaged, parts of the colon or rectum may need to be removed and reattached (bowel resection).
The choice of treatment depends on factors such as the patient’s age, overall health, severity of the prolapse, and the surgeon’s expertise. It’s essential to consult with a healthcare professional for a thorough evaluation and to determine the most appropriate treatment plan for rectal prolapse.
Harshad N Soni
MS, FIAGES- Consultant GI & Laparoscopic Surgeon
Kaizen Hospital