Kaizen Cancer Center

Cancer refers to any one of a large number of diseases characterized by the development of abnormal cells that divide uncontrollably and have the ability to infiltrate and destroy normal body tissue. Cancer often has the ability to spread throughout your body.
Cancer is the second-leading cause of death in the world.
Cancer develops when the body’s normal control mechanism stops working. Old cells do not die and instead grow out of control, forming new, abnormal cells. These extra cells may form a mass of tissue, called a tumor. Some cancers, such as leukemia, do not form tumors.
Cancer causes cells to divide uncontrollably. This can result in tumors, damage to the immune system, and other impairment that can be fatal.
Gastrointestinal (GI) cancer is a term for the group of cancers that affect the digestive system.
GI cancer is the most common form of cancer, affecting both men and women.
Signs and Symptoms of gastrointestinal cancer
- Poor appetite.
- Weight loss (without trying)
- Abdominal (belly) pain.
- Vague discomfort in the abdomen, usually above the navel.
- Feeling full after eating only a small meal.
- Heartburn or indigestion.
- Nausea.
- Vomiting, with or without blood.
Cancer of Esophagus
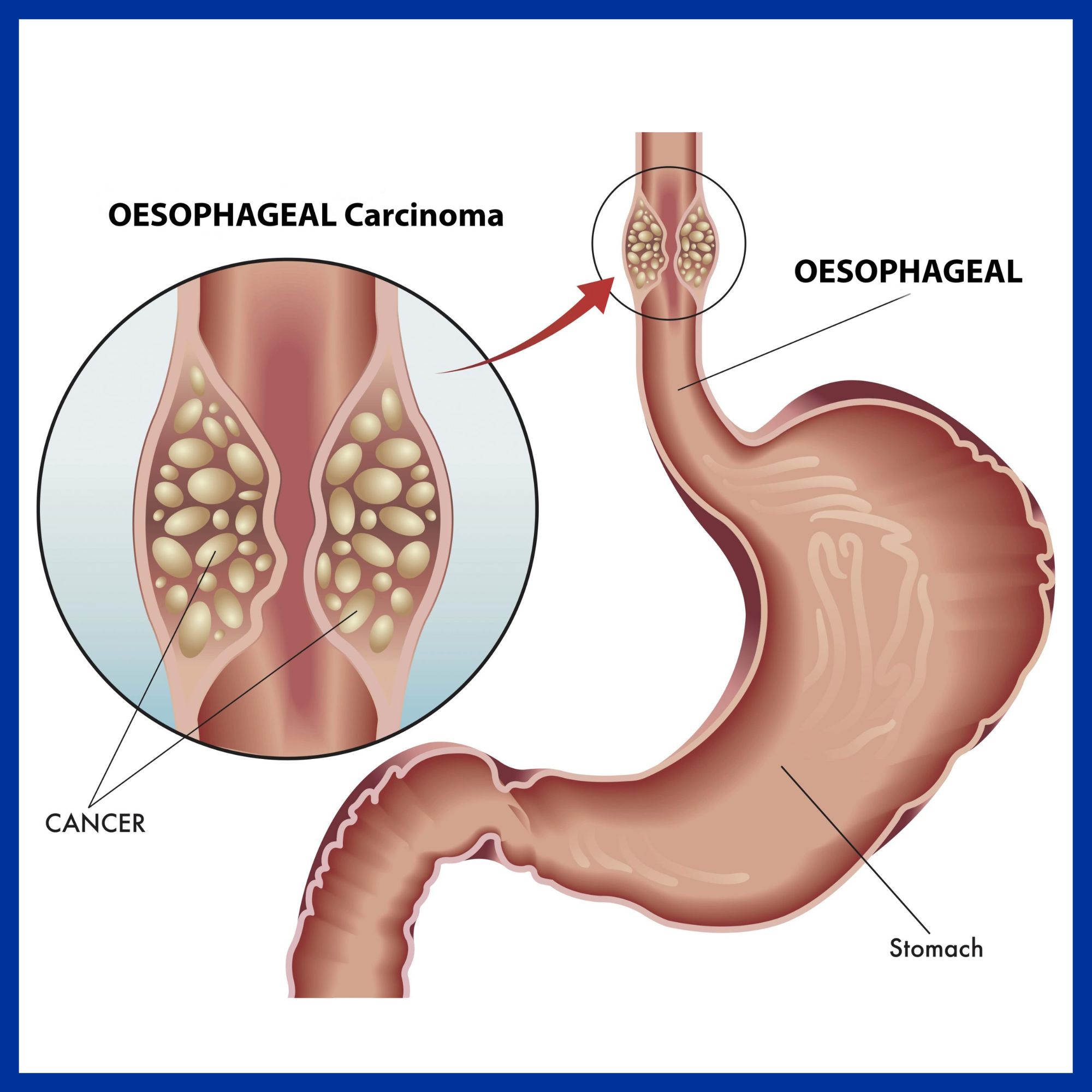
Signs and symptoms of Esophagus cancer
1. Difficulty in swallowing, initially with solid foods and later with softer foods and liquids.
2. Pain when swallowing (less common initially).
3. Weight loss, especially in cases of squamous-cell carcinoma.
4. Pain behind the breastbone or in the stomach region, often resembling heartburn.
5. Husky, raspy, or hoarse-sounding cough (result of the tumor affecting the recurrent laryngeal nerve).
6. Nausea and vomiting, regurgitation of food.
7. Increased risk of aspiration pneumonia.
8. Development of abnormal connections (fistulas) between the esophagus and trachea.
9. Coughing on drinking or eating in the presence of fistulas.
10. Vomiting of blood due to fragile tumor surface and bleeding.
11. Compression of local structures in advanced disease, leading to upper airway obstruction and superior vena cava syndrome.
12. Symptoms related to metastatic disease if cancer has spread, including jaundice, abdominal swelling (ascites), impaired breathing (pleural effusion), and dyspnea.
Causes
The two main types (i.e. squamous-cell carcinoma and adenocarcinoma) have distinct sets of risk factors or causes.
Squamous-Cell Carcinoma:
1. Tobacco: Smoking or chewing tobacco is a major risk factor.
2. Alcohol: Heavy alcohol consumption is another significant risk factor.
3. Synergistic Effect: The combination of tobacco and alcohol has a strong synergistic effect.
4. Dietary Exposure: High levels of dietary exposure to nitrosamines (found in tobacco smoke and certain foods) are relevant risk factors.
5. Dietary Patterns: Unfavorable dietary patterns involving nitrosamine exposure through processed and barbecued meats, pickled vegetables, and low intake of fresh foods.
6. Other Factors: Nutritional deficiencies, low socioeconomic status, poor oral hygiene, and chewing betel nut (areca) in Asia.
Adenocarcinoma:
1. Male Predominance: Adenocarcinoma is more common in men, occurring about 7 to 10 times more frequently.
2. Acid Reflux (GERD): Long-term erosive effects of acid reflux, known as gastroesophageal reflux disease (GERD), are strongly linked to adenocarcinoma.
3. Barrett’s Esophagus: Barrett’s esophagus can develop due to GERD, especially in men, and is associated with a higher risk of adenocarcinoma.
4. Obesity: Obesity and overweight are associated with an increased risk of adenocarcinoma, with abdominal obesity being particularly relevant.
5. Chronic Inflammation: Abdominal obesity stimulates GERD and has other chronic inflammatory effects, possibly contributing to the risk.
Diagnosis
Clinical evaluation
The diagnostic procedure for evaluating an occlusive tumor in the esophagus is typically done as follows:
1. Initial Evaluation: When an occlusive tumor is suspected, clinical evaluation may begin with a barium swallow or barium meal, but these are not definitive for diagnosis.
2. Primary Diagnostic Procedure: The diagnosis is best made through esophagogastroduodenoscopy (endoscopy). This procedure involves the insertion of a flexible tube with a light and camera down the esophagus to visually examine the esophageal wall. During endoscopy, biopsies may be taken from suspicious lesions for histological examination to determine if malignancy is present.
3. Staging Assessment: Additional testing is performed to estimate the tumor stage, typically using the TNM staging system. This includes:
– Computed Tomography (CT): CT scans of the chest, abdomen, and pelvis are used to assess whether cancer has spread to adjacent tissues or distant organs, particularly the liver and lymph nodes. CT scans are sensitive to detecting masses generally larger than 1 cm.
– Positron Emission Tomography (PET): PET scans are used to estimate the extent of the disease and are considered more precise than CT alone.
– Esophageal Endoscopic Ultrasound: This procedure provides staging information regarding the level of tumor invasion and the potential spread to regional lymph nodes.
4. Tumor Location: The location of the tumor is typically measured by the distance from the teeth. The esophagus, which is approximately 25 cm (10 inches) long, is commonly divided into three parts for location determination. Adenocarcinomas tend to occur nearer the stomach, while squamous cell carcinomas tend to occur nearer the throat. However, both types of tumors can arise anywhere along the length of the esophagus.
Prevention
Prevention includes stopping smoking or chewing tobacco. Overcoming addiction to areca chewing in Asia is another promising strategy for the prevention of esophageal squamous-cell carcinoma.
According to the National Cancer Institute, “diets high in cruciferous (cabbage, broccoli, cauliflower, Brussels sprouts) and green and yellow vegetables and fruits are associated with a decreased risk of esophageal cancer” Dietary fiber is thought to be protective, especially against esophageal adenocarcinoma.
Screening
People with Barrett esophagus (a change in the cells lining the lower esophagus) are at much higher risk and may receive regular endoscopic screening for the early signs of cancer. Because the benefit of screening for adenocarcinoma in people without symptoms is unclear, it is not recommended in the United States. Some areas of the world with high rates of squamous-carcinoma have screening programs.
Management
The treatment is determined by the cellular type of cancer (adenocarcinoma or squamous-cell carcinoma vs other types), the stage of the disease, the general condition of the patient, and other diseases present. Treatment should be managed by a multidisciplinary team covering the various specialities involved. Adequate nutrition needs to be assured, and adequate dental care is vital.
A number of types and combinations of surgery, chemotherapy, and radiotherapy, as well as other therapies, have been used over recent decades, but there has been no transformative improvement in outlook for patients equivalent to that seen in some other cancers.
Cancer of Stomach
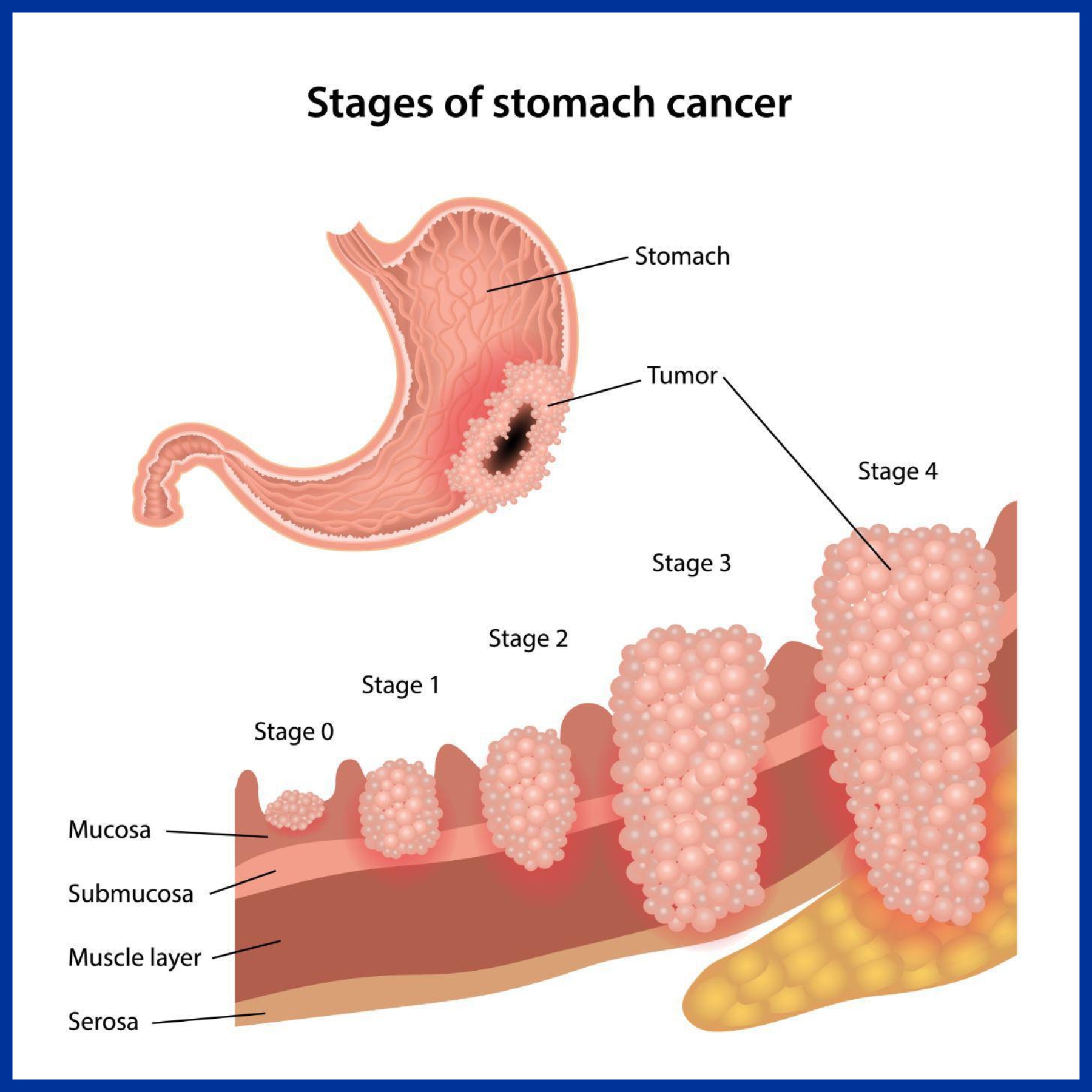
What causes stomach cancer?
A cancerous tumor starts from one abnormal cell. The exact reason why a cell becomes cancerous is unclear. It is thought that something damages or alters certain genes in the cell. These make the cell abnormal and multiply out of control.
Many people develop stomach cancer for no apparent reason. However, certain risk factors increase the chance that stomach cancer may develop. These include:
- Ageing: Stomach cancer is more common in older people. Most cases are in people over the age of 55.
- Anemia: Having a type of anemia called pernicious anemia, which causes a lack of vitamin B12, can slightly increase your risk of stomach cancer.
- Diet is probably a factor:
- oCountries such as Japan, where people eat a lot of salt, pickled and smoked foods, have a high rate of stomach cancer.
- oEating a lot of fruit and green vegetables can reduce the risk.
- Smoking: Smokers have a higher rate of stomach cancer compared with people who do not smoke.
- H Pylori: Long-term infection of the stomach lining with a bacterium called Helicobacter pylori seems to lead to a slightly higher risk of stomach cancer.
- Gender: Stomach cancer is twice as common in men as in women.
- If you have had part of your stomach removed in the past for any reason. For example, to treat a stomach ulcer or some other condition.
- Family history: For some cases, stomach cancer may run in the family. However, most cases of stomach cancer do not run in families and are not inherited.
- Blood group A: People who have this blood group have a slightly higher risk.
What are the symptoms of stomach cancer?
When a stomach cancer first develops and is small, it usually causes no symptoms. Some do not cause symptoms until they are quite advanced.
Initial symptoms may include:
- Pain or discomfort in the upper abdomen, especially after eating.
- Indigestion.
- Feeling sick, off food. Some people have a sense of fullness after eating.
- Weight loss and/or loss of appetite.
- You may pass blood out with your faeces. You may not notice bleeding if small amounts of blood pass out with your faeces. A lot of bleeding from the stomach can turn your faeces black.
As the cancer grows in the stomach, symptoms may become worse and may include:
- The same symptoms as above, but more severe.
- Feeling generally unwell and more tired than usual.
- Becoming anemic if the tumor regularly bleeds. This can cause you to become more tired than usual.
- The cancer growing very large and causing a blockage to food and drink.
If the cancer spreads to other parts of the body, various other symptoms can develop.
How is stomach cancer diagnosed and assessed?
Initial assessment and endoscopy
If a doctor suspects that you may have stomach cancer, he or she may examine you. The examination is often normal, especially if the cancer is at an early stage. Therefore, an endoscopy is usually arranged.
Biopsy – to confirm the diagnosis
A biopsy is when a small sample of tissue is removed from a part of the body. The sample is then examined under the microscope to look for abnormal cells.
Assessing the extent and spread
If you are confirmed to have stomach cancer, further tests may be done to assess if it has spread. For example, a barium meal X-ray, a CT scan, an MRI scan, an ultrasound scans laparoscopy or other tests.
What are the treatment options for stomach cancer?
Treatment options which may be considered include surgery, chemotherapy and sometimes radiotherapy.
Surgery
Removing the tumor may be curative if the cancer is in an early stage. The common operation is to cut out the affected part of the stomach.
Chemotherapy
Chemotherapy is a treatment of cancer by using anti-cancer medicines which kill cancer cells or stop them from multiplying. When chemotherapy is used in addition to surgery it is known as adjuvant chemotherapy.
Radiotherapy
Radiotherapy is a treatment which uses high energy beams of radiation which are focused on cancerous tissue. This kills cancer cells, or stops cancer cells from multiplying.
Chemoradiotherapy
In some cases a combination of chemotherapy and radiotherapy is offered, often as an addition to surgery. If you need to have this, it is usually done around the time of the operation.
Cancer of Liver
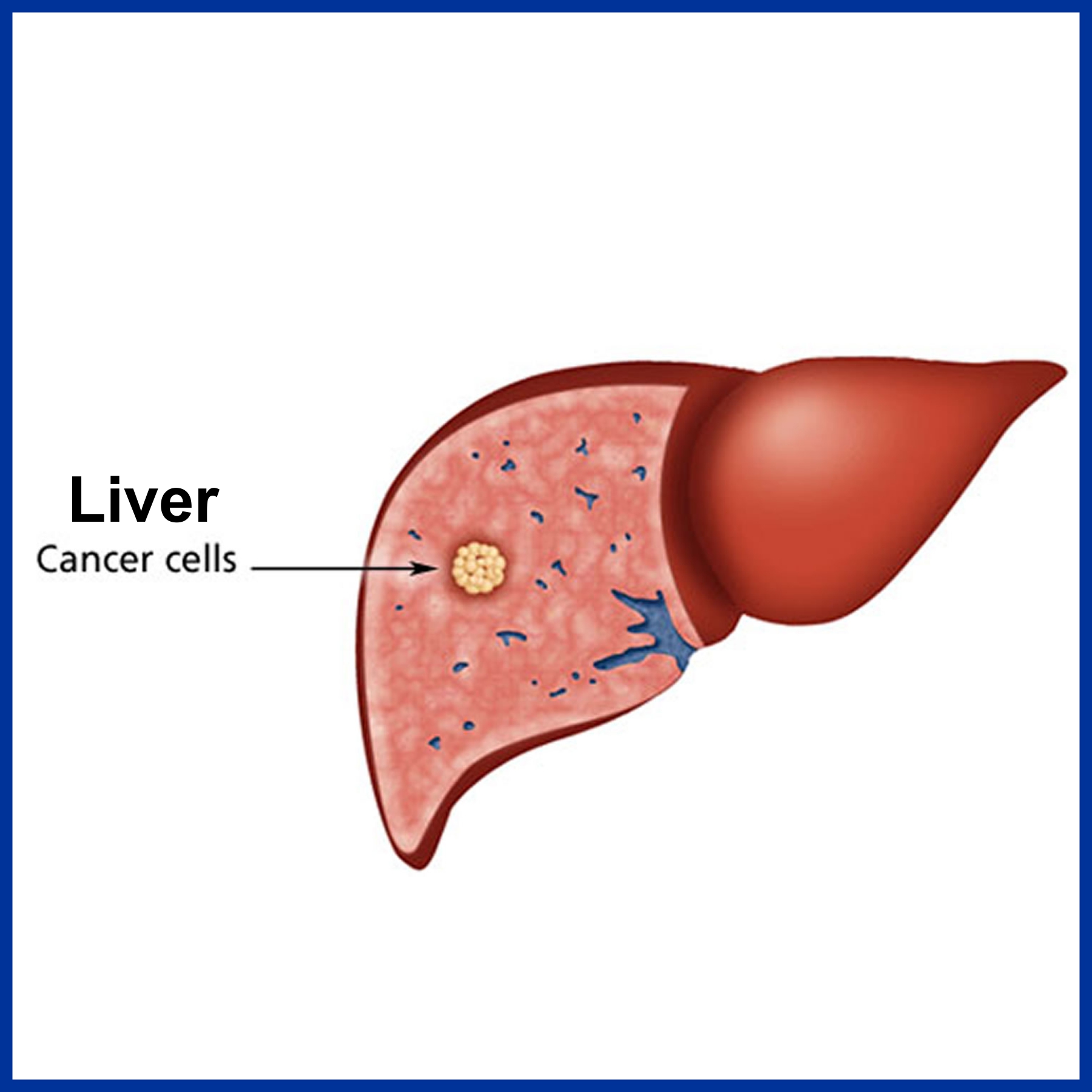
Primary liver cancer means that the cancer started (originated) in the liver. In the UK, primary liver cancer is uncommon. There are around 3,000 cases of primary liver cancer each year in the UK. It occurs most commonly in people aged over 65 years. However, worldwide, it is one of the most common cancers.
Secondary (metastatic) liver cancer means that a cancer which started in another part of the body has spread to the liver. Many types of cancer can spread to the liver. Most commonly, cancers of the bowel, pancreas, stomach, lung or breast. The
behavior, treatment and outlook of secondary liver cancers are often quite different to primary liver cancer.
There are different types of primary liver cancer which include:
- Hepatoma: This is the most common type (about 9 in 10 cases). It is sometimes called hepatocellular carcinoma (HCC). This type of cancer originates from a liver cell (hepatocyte) which becomes cancerous. (The bulk of the liver is made up from hepatocytes). A hepatoma most commonly develops as a complication of liver diseases such as cirrhosis (scarring of the liver) or types of hepatitis (liver inflammation).
- Fibrolamellar hepatoma is a rare subtype of hepatoma. It typically develops in a liver which was previously healthy.
- Cholangiocarcinoma: This is uncommon. It develops from cells which line the bile duct.
- Hepatoblastoma: This is a rare cancer which occurs in some young children.
- Angiosarcoma: This is rare. It develops from blood vessel cells within the liver.
What causes liver cancer?
A cancerous tumor starts from one abnormal cell. The exact reason why a cell becomes cancerous is unclear. It is thought that something damages or alters certain genes in the cell. These make the cell abnormal and multiply out of control.
Most people who develop a primary liver cancer have one or more of the following risk factors which seem to make liver cells more prone to becoming cancerous:
- Cirrhosis. This is a condition which causes scarring of the liver. It tends to progress slowly. In the UK, the common causes of cirrhosis are heavy alcohol drinking, and infection with hepatitis C. However, there are various other causes of
cirrhosis. Note: most people with cirrhosis do not develop liver cancer – it occurs in only a small number of people with cirrhosis. - Long-term infection with the hepatitis B or hepatitis C virus. It typically takes 20-30 years after first becoming infected to develop primary liver cancer. Infection with these viruses is not common in the UK, but it is becoming more common. However, these are common infections worldwide, particularly in Asia and Africa. Many young children in these areas are infected with the hepatitis B virus. This is why primary liver cancer is a common cancer in young adults in these areas of the world (developing 20-30 years after first being infected).
- Ingesting some poisons or toxins. For example, a known risk factor is a poison called aflatoxin which contaminates some foods (for example, mouldy peanuts), mainly in developing countries.
- Some conditions which cause persistent inflammation of the gut increase the risk slightly of developing a cholangiocarcinoma (an uncommon type of primary liver cancer) – for example, ulcerative colitis.
- There is some evidence that smoking can increase the risk
- A parasitic infection (liver fluke) which mainly occurs in Africa and Asia increases the risk of developing a cholangiocarcinoma.
What are the symptoms of liver cancer?
There may be no symptoms in the early stage of the disease. As the cancer grows, the first symptoms to develop may be quite vague and nonspecific. For example, feeling generally unwell, feeling sick (nausea), loss of appetite, weight loss and tiredness. Many people who develop primary liver cancer will already have symptoms associated with cirrhosis. If you already have cirrhosis and your health becomes worse quite quickly, the cause may be a liver cancer which has developed.
As the cancer develops further, more specific symptoms which may also develop include:
- Abdominal pain over the liver area.
- Jaundice. Jaundice is when you go yellow. You tend to first notice it when the whites of the eyes become yellow. It is due to a build-up of the chemical bilirubin which is made in the liver. This occurs if the bile duct becomes blocked by the
cancer. Bile and bilirubin cannot drain out from the liver and so leak into the bloodstream. - Itch (caused by the jaundice).
- Swelling of the abdomen. This can be due to the growing cancer itself. It may also be due to ascites which is fluid that builds up in the abdomen which occurs with various liver disorders.
How is cancer of the liver diagnosed and assessed?
Screening
Screening using ultrasound, and sometimes also a blood test for alpha-fetoprotein (AFP), at 6- to 12-month intervals, has been recommended for people at high risk of liver cancer. This includes people with liver cirrhosis associated with infection with hepatitis B or hepatitis C virus. This can detect liver cancer at an earlier stage and therefore improve the chance of successful treatment.
Initial assessment
If liver cancer is suspected, you are likely to have a number of tests. These aim to:
- Confirm that you have a cancer in the liver. Also, that the cancer is a primary liver cancer and not a secondary liver cancer.
- Assess the stage of the cancer. That is, how much of the liver is affected and whether the cancer has spread to other parts of the body.
- Assess the state of your liver function and your general health.
- Therefore, a range of tests are usually needed. They may include:
- Scans such as ultrasound scan, CT scan or MRI scan. These can help to show the exact location and extent of the cancer.
- A liver biopsy. This is usually done to confirm the type of cancer. A biopsy is when a small sample of tissue is removed from a part of the body.
- The sample is then examined under the microscope to look for abnormal cells.
- Blood tests help to assess the liver function and your general health.
- Other tests may be done if the above do not clarify the situation. For example, a laparoscopy is sometimes done. This is a small operation to look inside the abdomen with a flexible telescope.
What are the treatment options for liver cancer?
The main treatments used for liver cancer are surgery and chemotherapy. Other techniques are sometimes used. The treatment advised in each case depends on various factors such as:
- The exact site of the primary tumour in the liver.
- The stage of the cancer (how large the cancer is and whether it has spread). See also separate leaflet called Staging and grading cancer.
- Your general health. In particular, the general state of your liver and liver function (many people with primary liver cancer also have poor liver function due to cirrhosis).
Surgery
Surgery which aims to cure the cancer is an option in some cases. If the cancer is small, has not spread outside the liver, and the rest of the liver is healthy, then it may be possible to cut out the part of the liver which contains the cancer. Healthy liver tissue will regrow to its full size within a few weeks if a section of liver is cut out. However, this operation is not suitable if your liver is damaged with severe cirrhosis (which is the case in many people with primary liver cancer). A liver transplant is another option, but again only suitable for a small number of cases.
Surgery also has a role in palliative care. For example, if jaundice is severe, it may be possible to relieve the blockage of the bile by inserting a stent.
This is a narrow tube which allows the bile to drain into the gut. Another example is to ease ascites (fluid in the abdomen) if it is severe. The ascites can be drained by inserting a tube through the wall of the abdomen.
Chemotherapy
Chemotherapy is a treatment which uses anti-cancer medicines to kill cancer cells, or to stop them from multiplying. It is not likely to be curative for primary liver cancer, but may shrink the tumour down to slow the progression of the disease.
There are new medicines being developed for the treatment of liver cancer. For example, sorafenib is a type of medicine called a multi-targeted kinase inhibitor. It interferes with the growth of cancer cells. Research has shown that sorafenib can be beneficial for people with advanced hepatocellular carcinoma. However, sorafenib is not currently recommended by the National Institute for Health and Clinical Excellence (NICE) for the treatment of people with advanced hepatocellular carcinoma.
Other treatments
Various other treatment techniques are sometimes used. For example:
- Alcohol ablation. Ablation means to destroy. For this treatment, alcohol is injected into the tumour. The alcohol kills cancer cells.
- Radiofrequency ablation. For this treatment, a needle is inserted into the tumour. High-intensity radio waves or laser light are then passed hrough the needle. This heats the cancer cells and kills them.
- Cryotherapy. For this treatment, a small metal object filled with liquid nitrogen is placed into the tumour. The liquid nitrogen makes it very cold which destroys cancer cells.
- Chemoembolisation. For this treatment, medicines used for chemotherapy are mixed with another oily chemical. The mixture is then injected into branches of the liver artery (hepatic artery) which are supplying the tumour with blood. The oily chemical helps to hold the chemotherapy medicines longer in the liver, and make them more effective in killing cancer cells.
- Radiotherapy.This is a treatment which uses high-energy beams of radiation which are focused on cancerous tissue. This kills cancer cells, or stops cancer cells from multiplying. Radiotherapy is not often used for primary liver cancers apart
form the uncommon cholangiocarcinoma type of cancer.
What is the prognosis?
Overall, the outlook is poor. Many people who develop primary liver cancer are already in poor health with cirrhosis. The best chance of a cure is with surgery when the cancer is small, has not spread from the liver, and the rest of your liver is relatively healthy. However, this situation only occurs in a minority of cases. The various other treatments described above may delay the progression of the disease, but are not often curative.
Cancer of Gallbladder
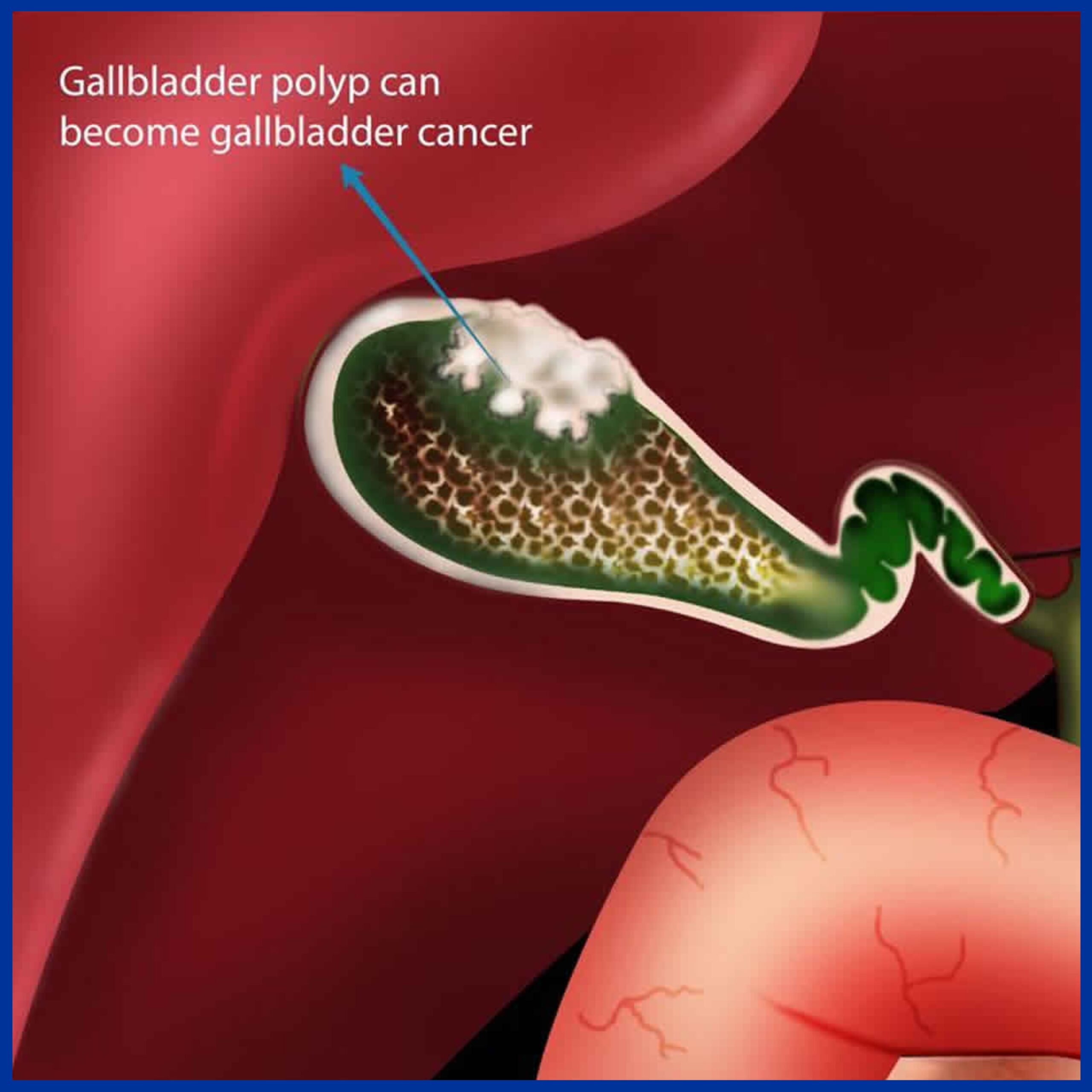
American Indians and Hispanics. If it is diagnosed early enough, it can be cured by removing the gallbladder, part of the liver and associated lymph nodes. Most often it is found after symptoms such as abdominal pain, jaundice and vomiting occur, and it has spread to other organs such as the liver. The incidence of gall bladder cancer is increasing in China as well as north central India.
It is a rare cancer that is thought to be related to gallstones building up, which also can lead to calcification of the gallbladder, a condition known as porcelain gallbladder. Porcelain gallbladder is also rare. Some studies indicate that people with porcelain gallbladder have a high risk of developing gallbladder cancer, but other studies question this. The outlook is poor for recovery if the cancer is found after symptoms have started to occur, with a 5-year survival rate close to 3%.
- Gender: twice more common in women than men, usually in seventh and eighth decades.
- Obesity increases the risk for gallbladder cancer.
- Chronic cholecystitis and cholelithiasis.
- Chronic typhoid infection of gallbladder. Chronic salmonella typhi carriers have 3 to 200 times higher risk of gallbladder cancer than non-carriers and 16% lifetime risk of development of cancer.
- Various single nucleotide polymorphisms (SNPs) have been shown to be associated with gallbladder cancer. However, existing genetic studies in GBC susceptibility have so far been insufficient to confirm any association.
Signs and symptoms
- Steady pain in the upper right abdomen
- Weakness
- Loss of appetite
- Weight loss
- Jaundice and vomiting due to obstruction
Early symptoms mimic gallbladder inflammation due to gallstones. Later, the symptoms may be that of biliary and stomach obstruction.
Disease course
Most tumors are adenocarcinomas, with a small percent being squamous cell carcinomas. The cancer commonly spreads to the liver, bile duct, stomach, and duodenum.
Diagnosis
Early diagnosis is not generally possible. People at high risk, such as women or Native Americans with gallstones, are evaluated closely. Trans-abdominal ultrasound, CT scan, endoscopic ultrasound, MRI, and MR cholangio-pancreatography
(MRCP) can be used for diagnosis. A biopsy is the only certain way to tell whether the tumors growth is malignant or not.
Treatment
The most common and most effective treatment is surgical removal of the gallbladder (cholecystectomy) with part of liver and lymph node dissection. However, with gallbladder cancer’s extremely poor prognosis, most patients will die by one year following the surgery. If surgery is not possible, endoscopic stenting of the biliary tree can reduce jaundice and a stent in stomach may relieve vomiting. Chemotherapy and radiation may also be used with surgery. If gall bladder cancer is
diagnosed after cholecystectomy for stone disease, reoperation to remove part of liver and lymph nodes is required in most cases. When it is done as early as possible, patients have the best chance of long term survival and even cure.
Cancer of Bile Duct
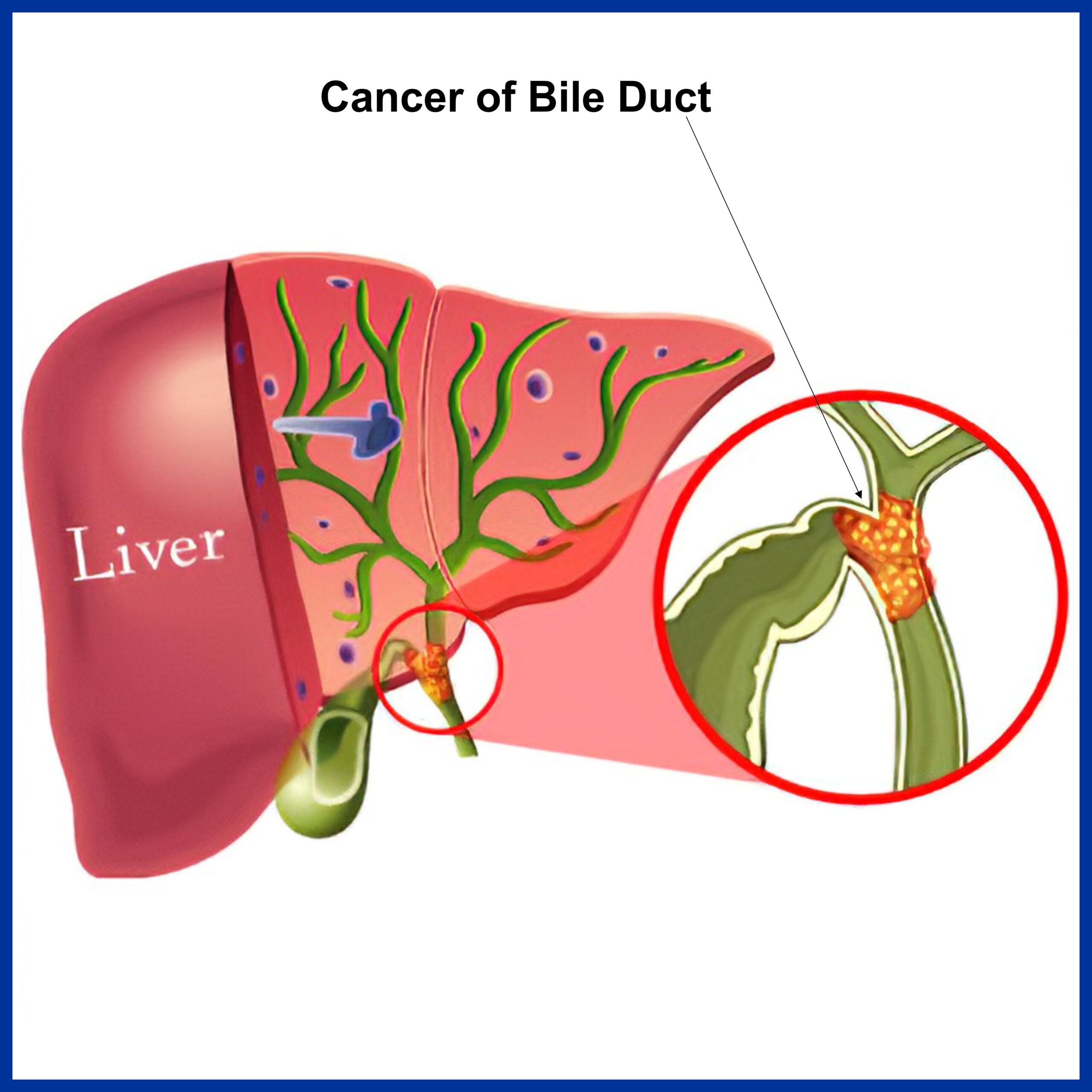
Causes
- Certain diseases of the liver or bile ducts- Primary sclerosing cholangitis ,Bile duct stones, Choledochal cysts,Liver fluke infectionsCirrhosis,Infection withhepatitis B virus or hepatitis C virus
- Inflammatory bowel disease
- Older age
- Obesity
- Family history
- Diabetes
- Alcohol
- Smoking
- Pancreatitis (inflammation of the pancreas)
- Infection with HIV (the virus that causes AIDS)
Symptoms
- Abnormal liver function tests,Jaundice
- Abdominal pain
- Generalized itching
- Weight loss
- Fever
- Changes in stool or urine colour
Diagnosis
- Blood Test
- Biopsy
- CT Scan
- ERCP
Treatment
- Surgery to remove the bile duct, and sometimes part of the liver
- Chemotherapy
- Radiation
- Stent placement
Complication
- Liver Failure
- Pneumonia
Cancer of Duodenum
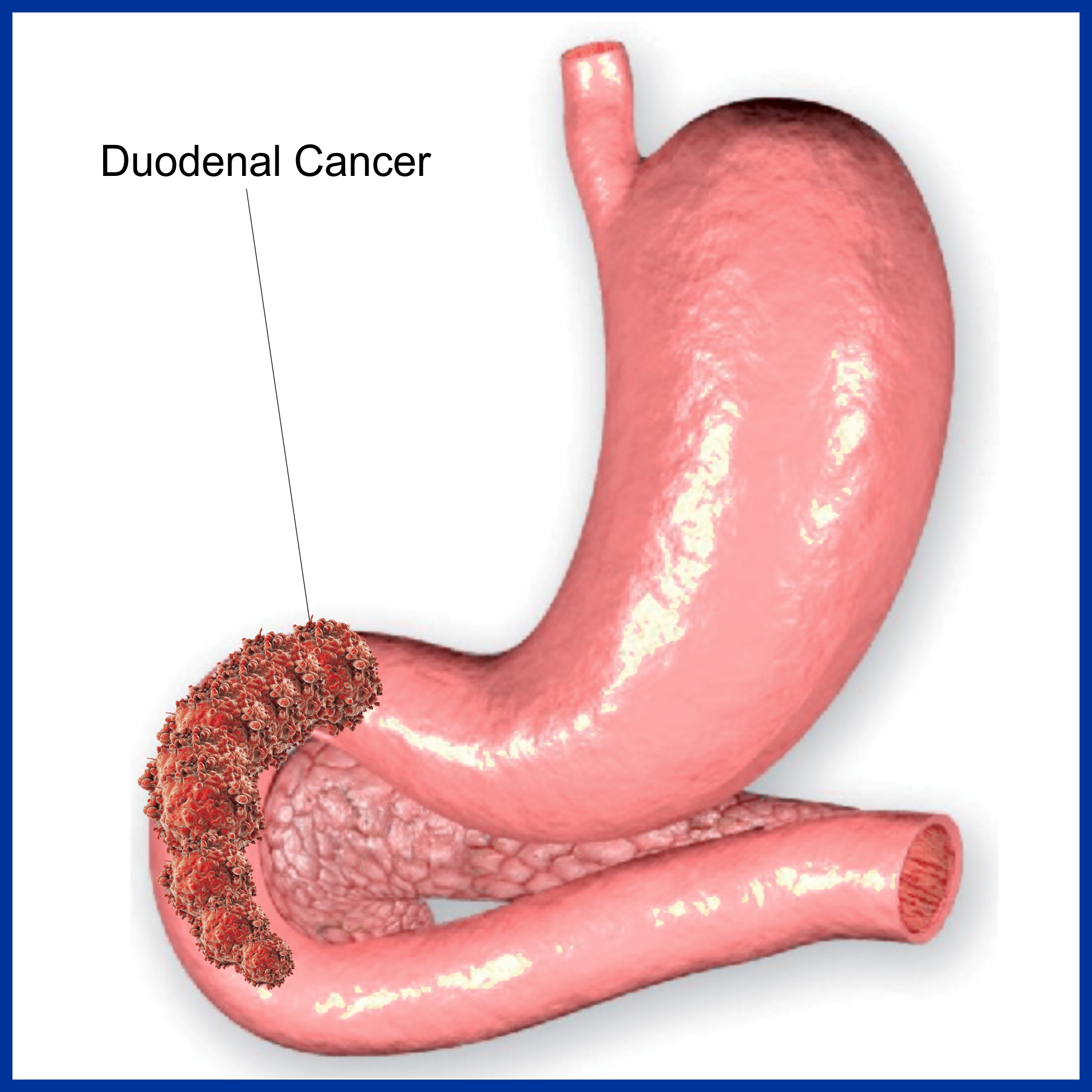
Duodenal cancer is a cancer of first part of the intestine called duodenum, which is a vital organ of digestive tract where bile juice, pancreatic juice and gastric juice are mixed and act on food material.
Risk Factors
- High Fat Diet
- Crohn’s disease
- Celiac disease
- Duodenal ulcer
- Juvenile polyposis syndrome
- Familial adenomatous polyposis (FAP)
- Muir -Torre syndrome- inherited disease caused due to genetic defect.
- Peutz-Jeghers syndrome – Inherited autoimmune disease.
Symptoms
- Heart burn, regurgitation
- Nausea, vomiting
- Bloating
- Weight loss
- Fatigue, generalised weakness
- Abdominal pain
- Melaena
Investigations
- CT Scan
- X Ray Abdomen
- UGI Endoscopy with biopsy
Treatment
- Treatment depends on patient’s age, health status and cancer stage.
- Surgery
- Chemotherapy
Cancer of Pancreas
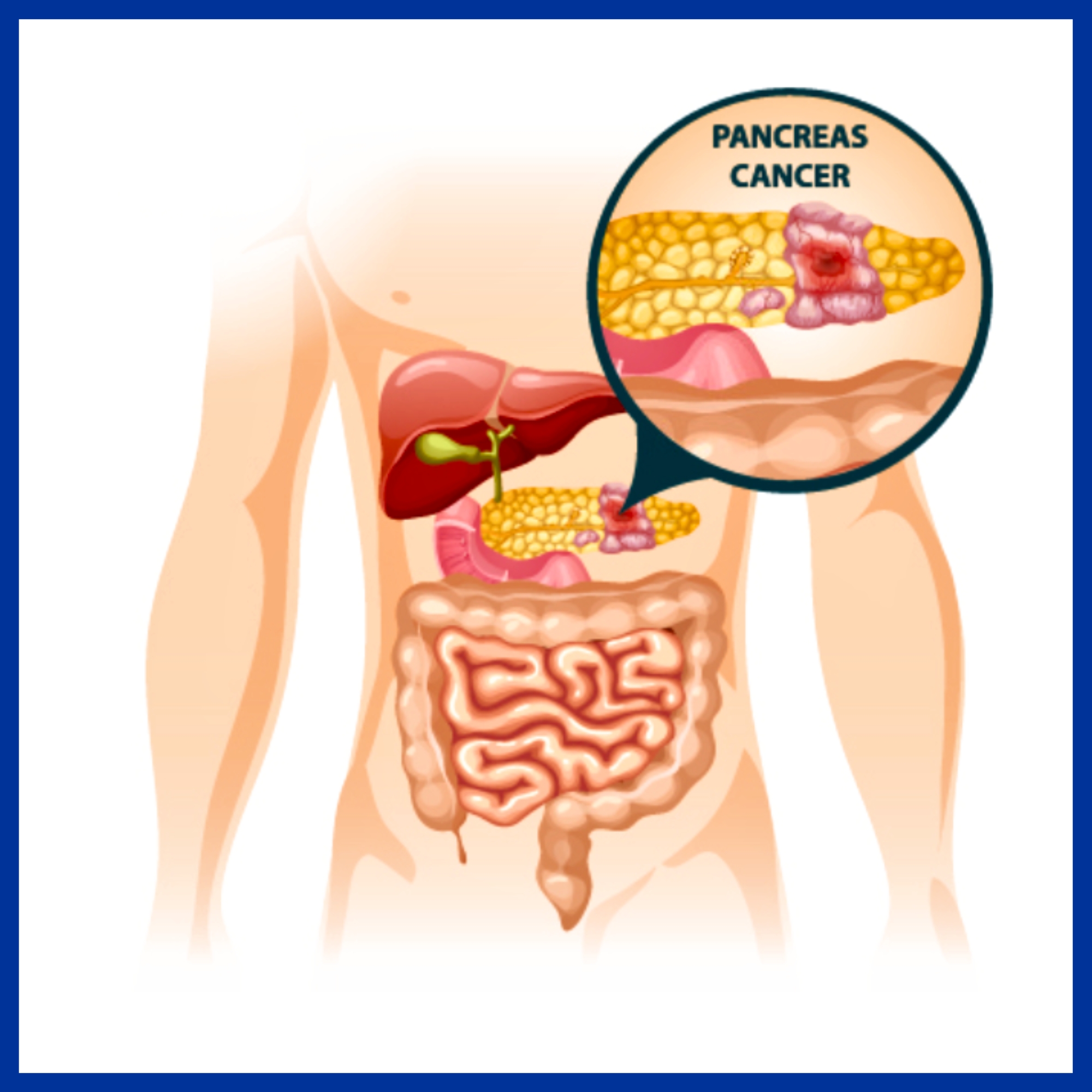
Pancreatic cancer is relatively uncommon. There are several types of pancreatic cancer, but more than 9 in 10 cases are ductal adenocarcinomas.
Ductal adenocarcinoma of the pancreas
This type of cancer develops from a cell which becomes cancerous in the pancreatic duct. This multiplies and a tumor then develops in and around the duct. As the tumor enlarges:
- It can block the bile duct or the main pancreatic duct. This stops the drainage of bile and/or pancreatic fluid into the duodenum.
- It invades deeper into the pancreas. In time it may pass through the wall of the pancreas and invade nearby organs such as the duodenum, stomach or liver.
- Some cells may break off into the lymph channels or bloodstream. The cancer may then spread to nearby lymph nodes or spread to other areas of the body (metastasis).
Other types of pancreatic cancer
There are some rare types of cancer which arise from other types of cells within the pancreas. For example, cells in the pancreas that make insulin or glucagon can become cancerous (insulinomas and glucagonomas). These behave differently to ductal adenocarcinoma. For example, they may produce too much insulin or glucagon, which can cause various symptoms.
What causes pancreatic cancer?
A cancerous tumor starts from one abnormal cell. The exact reason why a cell becomes cancerous is unclear. It is thought that something damages or alters certain genes in the cell. This makes the cell abnormal and multiplies out of control.
Many people develop cancer of the pancreas for no apparent reason. However, certain risk factors increase the chance that pancreatic cancer may develop. These include:
- Ageing: It is more common in older people. Most cases are in people aged over 60.
- Smoking
- Diet: Eating a diet high in fat and meat seems to increase the risk.
- Obesity
- Chronic pancreatitis: persistent inflammation of the pancreas. Most cases of chronic pancreatitis are due to drinking a lot of alcohol. There are other less common causes.
- Diabetes
- Chemicals: Heavy exposure at work to certain pesticides, dyes and chemicals used in metal refining may increase the risk.
Genetic and hereditary factors:
Most cases of pancreatic cancer do not run in families. However, some families have a higher incidence of pancreatic cancer than average. It is thought that about 1 in 10 pancreatic cancers are due to inheriting an abnormal gene. See your doctor if you are concerned that pancreatic cancer is common in your family. You may be offered screening tests with the aim of detecting pancreatic cancer at an early stage when the chance of a cure is high.
What are the symptoms of pancreatic cancer?
Symptoms of a blocked bile duct
In about 7 in 10 cases the tumor first develops in the head of the pancreas. A small tumor often causes no symptoms at first. As the tumor grows it tends to block the bile duct. This stops the flow of bile into the duodenum which leads to:
- Jaundice
- Dark urine – caused by the jaundiced blood being filtered by the kidneys
- Pale faeces – as the faeces contain no bile which causes their normal brown color
- Generalized itch caused by the bile in the bloodstream
Pain is often not a feature at first. Therefore a painless jaundice that becomes worse is often the first sign of pancreatic cancer. Nausea and vomiting are also fairly common symptoms.
Other symptoms
As the cancer grows in the pancreas, further symptoms that may develop include:
- Pain in the upper abdomen. Pain can also pass through to the back.
- You may feel generally unwell and lose weight. These symptoms are often the first to develop if the cancer develops in the body or tail of the pancreas (when the bile duct is not blocked).
- You may not digest food very well, as the amount of pancreatic fluid will be reduced. This can cause smelly pale faeces and weight loss.
- Rarely, diabetes develops if nearly all the pancreas is damaged by the tumor.
- Rarely, a tumor can trigger inflammation of the pancreas – acute pancreatitis. This can cause severe abdominal pain.
If the cancer spreads to other parts of the body, various other symptoms can develop.
How is pancreatic cancer diagnosed and assessed?
Initial assessment
There are many causes of jaundice and of the other symptoms listed above. For example, a blocked gallstone or hepatitis (liver inflammation). Therefore, some initial tests are usually arranged if you develop jaundice or the other symptoms listed above. Typically, these include an ultrasound scan of the abdomen and various blood tests. These initial tests can usually give a good idea if the cause of jaundice is a blockage from the head of the pancreas.
Assessing the extent and spread
If you are confirmed to have pancreatic cancer, or it is strongly suspected from the initial tests, then further tests may be done to assess if it has spread. For example:
- A CT scan (computerised tomography) is a commonly used test to assess pancreatic cancer. It is a specialised X-ray test that can give quite clear pictures of the inside of your body.
- An MRI scan is sometimes done. MRI stands for magnetic resonance imaging. An MRI scan uses a strong magnetic field and radio waves to create computer pictures of tissues, organs and other structures inside your body.
- An endoscopic ultrasound (EUS). An endoscope (gastroscope) is a thin, flexible, telescope. It is passed through the mouth, into the esophagus and stomach and on into the duodenum. The endoscope contains fiber optic channels which allow light to shine down so the doctor or nurse can see inside. Some endoscopes are fitted with a tiny ultrasound scanner at their tip, which can obtain pictures of structures behind the gut, such as the pancreas.
- Chest X-ray
- Laparoscopy This is a procedure to look inside your abdomen by using a laparoscope. A laparoscope is like a thin telescope with a light source. It is used to light up and magnify the structures inside the abdomen. A laparoscope is passed into the abdomen through a small incision (cut) in the skin.
Biopsy
A biopsy is when a small sample of tissue is removed from a part of the body. The sample is then examined under the microscope to look for abnormal cells. If a biopsy is thought to be needed then one way to get a sample from the pancreas is to take the biopsy sample when you have an endoscopy. This is done by passing a thin grabbing instrument down a side channel of the endoscope. Alternatively, sometimes a biopsy is done at the same time as having a scan. It can take two weeks for the result of a biopsy.
What are the treatment options for pancreatic cancer?
Treatment options that may be considered include surgery, chemotherapy and radiotherapy. The treatment advised for each case depends on various factors such as the stage of the cancer (how large the cancer is and whether it has spread), and your general health.
Surgery
If the cancer is at an early stage, then there is a modest chance that surgery can be curative. (An early stage means a small tumor which is confined within the pancreas and has not spread to the lymph nodes or other areas of the body).
- If the tumor is in the head of the pancreas then an operation to remove the head of the pancreas may be an option. This is a long and involved operation, as the surrounding structures such as the duodenum, stomach, bile duct, etc, need to be rearranged once the head of the pancreas is removed.
- If the tumor is in the body or tail of the pancreas then removal of the affected section of the pancreas is sometimes an option.
The reason why the chance of cure is only modest is because in a number of cases thought to be in an early stage, some cells have already spread to other parts of the body but are not yet detectable by scans or other staging tests. In time they grow into secondary tumors.
If the cancer is at a later stage then surgery is not an option to cure the disease. Some surgical techniques may still have a place to ease symptoms. For example, it may be possible to ease jaundice caused by a blocked bile duct. A bypass procedure may be used, or a stent may be inserted into the bile duct. (A stent is a small rigid tube made of plastic or metal which aims to keep a duct or channel open. It is usually inserted by instruments attached to an endoscope.)
Chemotherapy
Chemotherapy is a treatment of cancer by using anti-cancer medicines which kill cancer cells or stops them from multiplying. When chemotherapy is used in addition to surgery it is known as adjuvant chemotherapy. For example, following surgery you may be given a course of chemotherapy. This aims to kill any cancer cells which may have spread away from the primary tumor.
Radiotherapy
Radiotherapy is a treatment which uses high-energy beams of radiation which are focused on cancerous tissue. This kills cancer cells, or stops cancer cells from multiplying. See separate leaflet called Radiotherapy for more details. Radiotherapy is not commonly used to treat pancreatic cancer.
What is the prognosis?
If a pancreatic cancer is diagnosed and treated at an early stage then there is a modest chance of a cure with surgery. As a rule, the smaller the tumor, and the earlier the tumor is diagnosed, the better the outlook. Some tumors which develop in the head of the pancreas are diagnosed very early, as they block the bile duct and cause jaundice fairly early on. This obvious symptom is then investigated and surgery to remove a small tumor may be curative.
However, most pancreatic cancers are advanced before they cause symptoms and are diagnosed. A cure is unlikely in most cases. However, treatment may slow down the progression of the cancer.
Periampullary Cancer
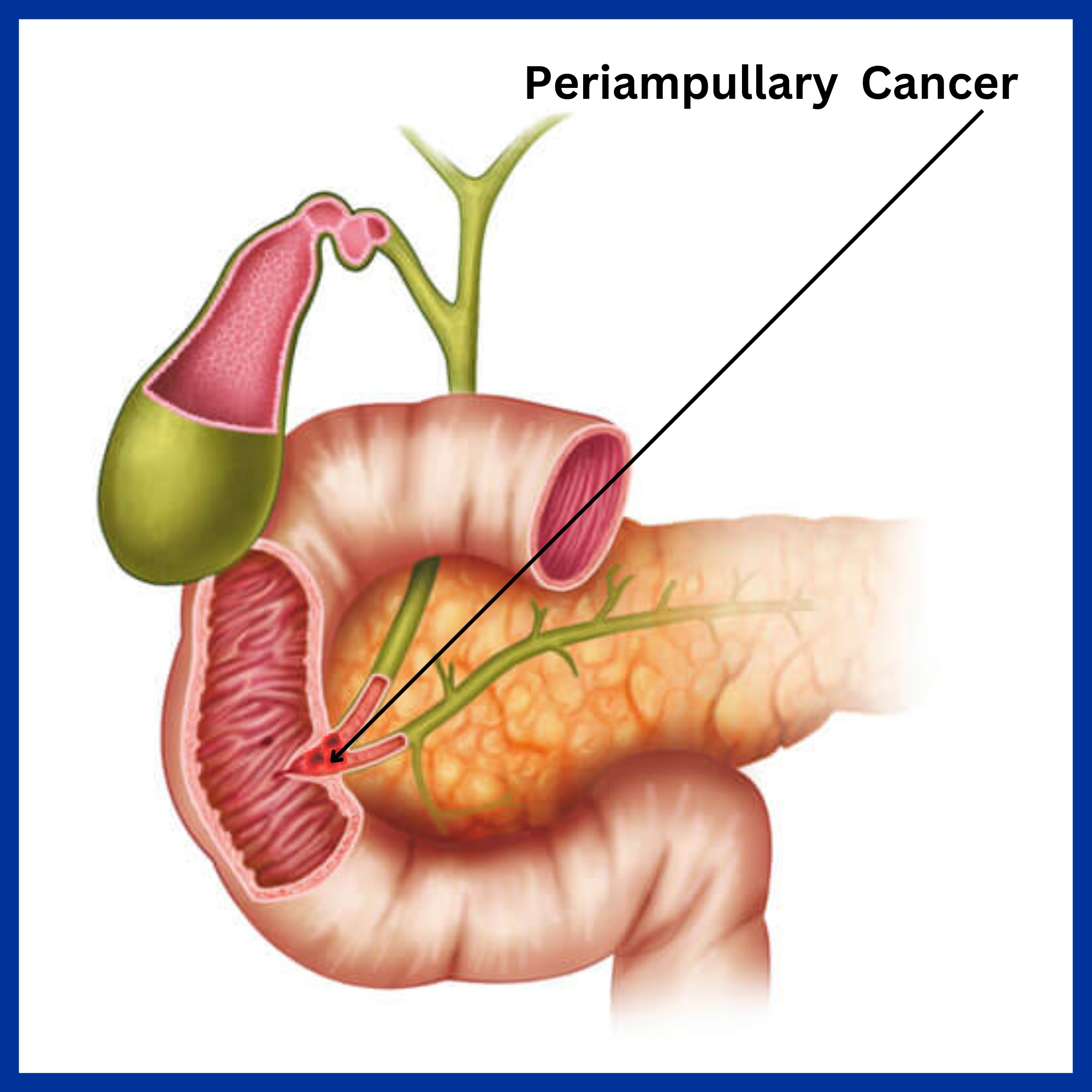
Causes
- Genetics, bile duct diseases,
Symptoms
- Intermittent or persistent jaundice
- Abdominal pain
- Backache
- Acute Pancreatitis
- Nausea, vomiting
- Pruritus
- Anorexia
- Cachexia
- Anaemia
- Fever
- Diarrhoea
Diagnosis
- CBC
- CEA, CA 19-9
- LFT
- Urine R/M
- USG Abdomen
- CT Scan
- EUS with biopsy
- MRCP (Magnetic Resonance Cholangiopancreatography)
- Chest X Ray
Treatment
- Surgery – Whipple procedure in case of large tumour – the lower half of the stomach, gallbladder, distal common bile duct, head of the pancreas, the upper parts of the small intestines and regional lymph nodes are removed. The remaining part of the stomach, biliary tree, and pancreas are attached to the cut end of the small intestine.
- Biliary stentsmay be placed endoscopically or through a skin incision to relieve the jaundice caused due to obstruction following the cancer.
Cancer of Small Intestine

- Age- More commonly seen in age groups above 60.
- Sex- More in males.
- Smoking
- Alcohol
- Celiac Disease
- Crohn’s Disease
- Exposure to radiation
- Cystic Fibrosis
- Koch’s
- Hamartoma
- Fistulous diseases
Symptoms
- Abdominal pain
- Anorexia
- Cachexia
- Anaemia
- Weakness and fatigue
- Nausea, vomiting
Diagnosis
- Medical history and physical exam
- CBC
- CT Scan
- Upper GI Endoscopy
- Colonoscopy
- Barium follow through
- Enteroclysis
- Barium enema
- Capsule endoscopy
- Double-balloon enteroscopy (endoscopy)
Treatment
- Treatment depends on patient’s age, health status and cancer stage.
- Surgery
- Chemotherapy
- Radiotherapy
Cancer of Large Intestine
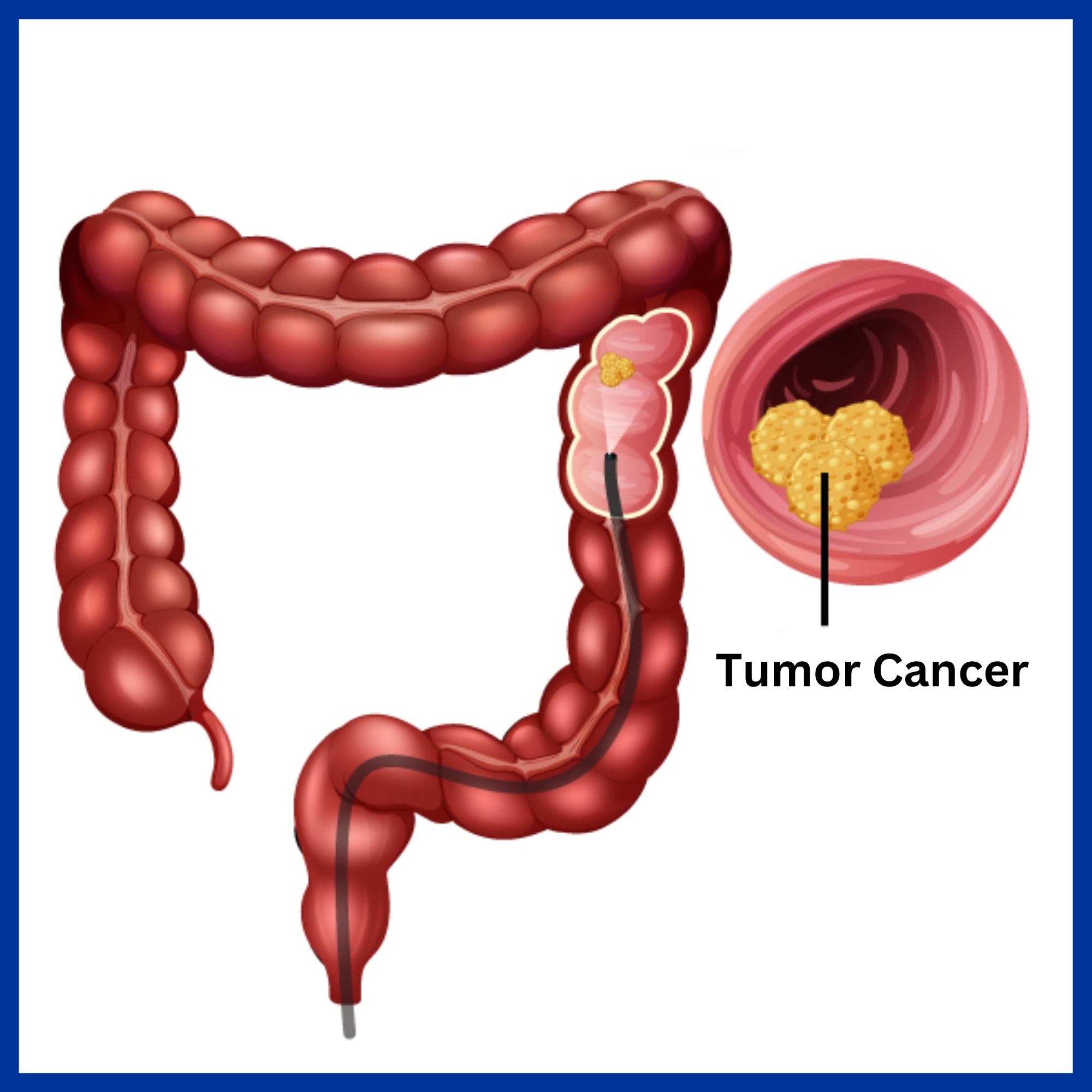
Ca colon means development of cancer in the colon.
Stages of Colon Cancer
- Stage I – Cancer limited to the superficial lining (mucosa) of the colon or rectum but hasnt spread beyond the colon wall or rectum.
- Stage II – Cancer grown into or through the wall of the colon or rectum but hasn’t spread to nearby lymph nodes.
- Stage III – Cancer has spread to nearby lymph nodes but not affectingthe other parts of body.
- Stage IV – Cancer has spread to other organs such as liver or lungs.
Risk factors
Older age- Age above 50.
Race – African-Americans have a greater risk of colon cancer.
Family history of colorectal cancer or polyp.
Inflammatory intestinal conditions – Ulcerative colitis or Crohn’s Disease.
GeneticDisorders – Familial adenomatous polyposis (FAP) and Hereditary
non polyposis colorectal cancer (HNPCC), which is also known as Lynch syndrome.
Diet– Diet which is low in fibre and high in fat and red, processed meat.
Sedentary lifestyle
Diabetes
Obesity
Smoking
Alcohol
Radiation therapy directed at abdomen for treating previous cancers.
Symptoms
- Diarrhoea or constipation or a change in the consistency of stool.
- Blood in stool.
- Abdominal cramps or pain.
- Feeling of inomplete evacuation
- Weakness or fatigue
- Weight loss
Diagnosis
- Colonoscopy with Biopsy
- CECT Abdomen + Pelvis
- Colon Cancer Staging – To know how much the tumour has spread whether the lymph nodes are involved or not and the extent of metastasis.
Treatment
If cancer is in a very early stage or localised in a polyp, it can be removed during colonoscopy.
Polyps that can not be removed during colonoscopy may be removed using laparoscopic surgery. In this procedure, surgeon performs the operation through key hole incisions inabdominal wall, by inserting instruments with attached cameras that display the colon on a video monitor.
Stage II Cancer-Partial colectomy – the part ofcolon that contains the cancer, along with a margin of normal tissue on either side of the cancer, is removed. Nearby lymph nodes are also removed and tested for cancer.
If the cancer is at the outlet ofrectum, a permanent or temporary colostomy is done. In this surgery, an opening is created in the wall of abdomen, from the remaining portion of bowel, for the elimination of body waste into a special
bag, which is known as colostomy bag, which if healed, is removed after 1 month. In some cases, the colostomy may be permanent.
Cancer of Appendix
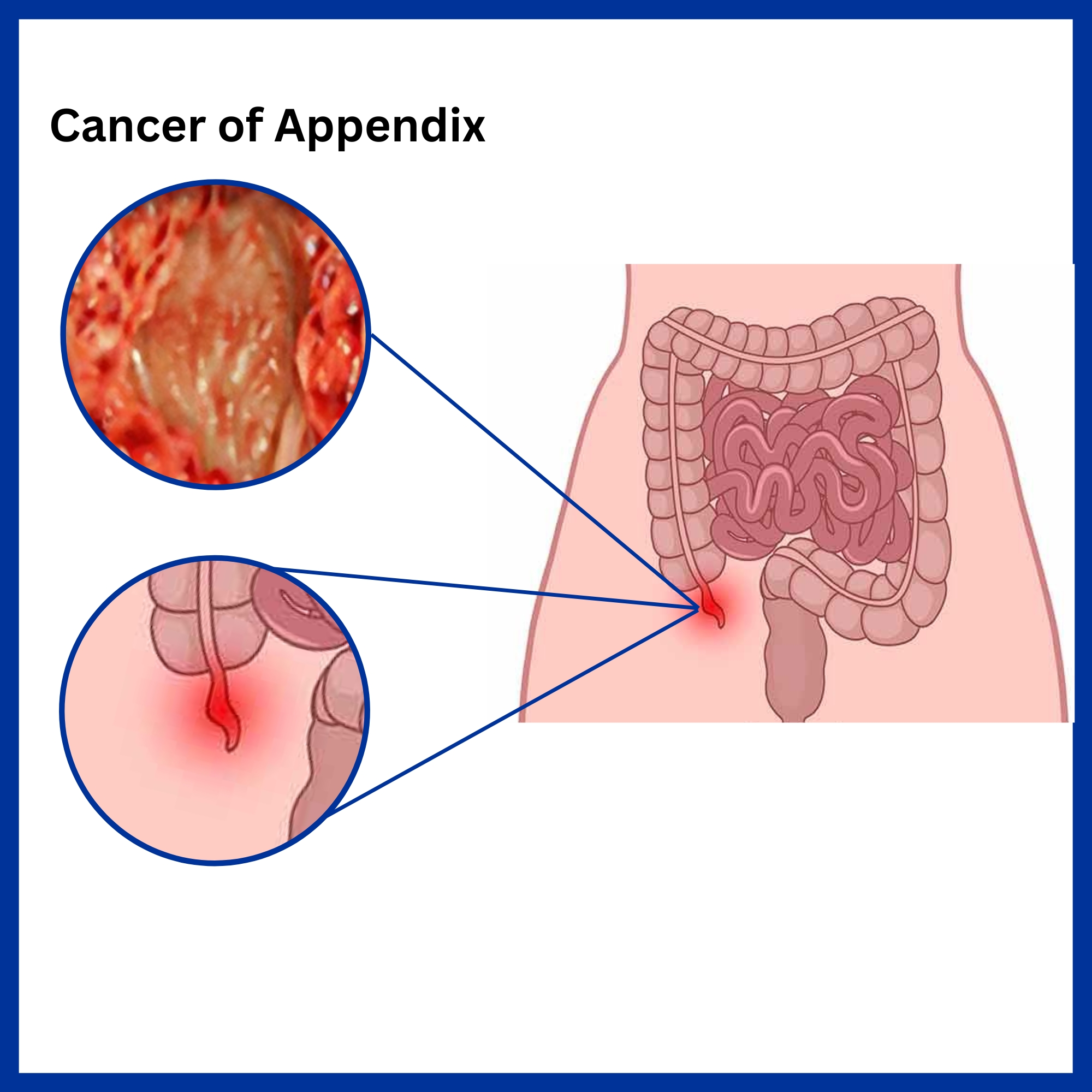
Types of Appendix Cancer
- Carcinoid tumours
- Non-carcinoid tumours
- Pseudomyxoma peritonei (PMP)
- Adenocarcinoid tumours
Symptoms
- Abdominal distention
- Acute or chronic abdominal pain
- Lower right abdominal discomfort
- Bowel obstruction
- Pelvic discomfort
Diagnosis
- CT or CAT (Computed Axial Tomography) scan
- MRI (Magnetic Resonance Imaging) scan
- PET (Positron Emission Tomography) scan
Treatment
- Surgery, chemotherapy
Cancer of Rectum
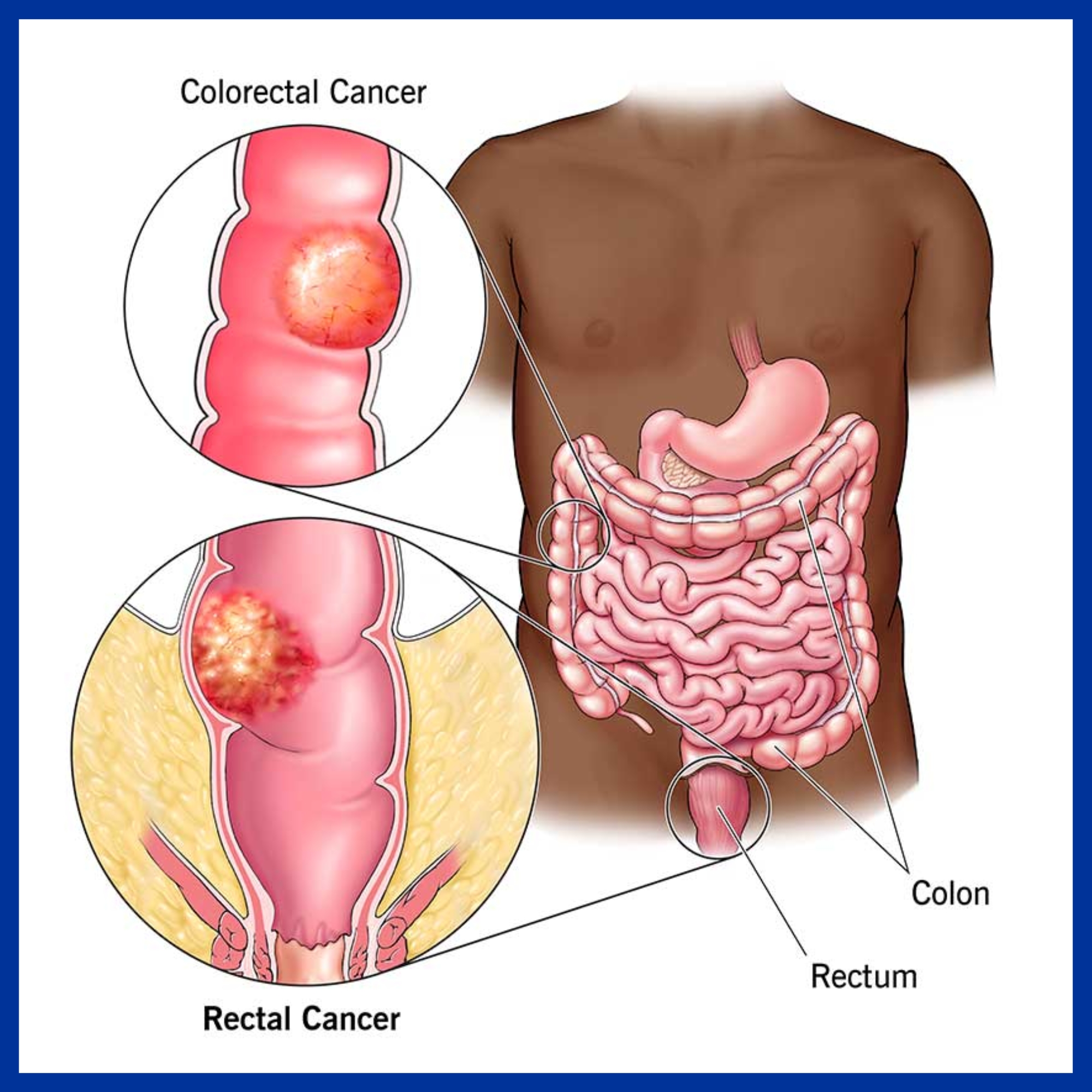
Causes
- Increasing age
- Smoking
- Family history of colon or rectal cancer
- High-fat diet and/or a diet mostly from animal sources
- Personal or family history of polyps or colorectal cancer
- Inflammatory bowel disease
Symptoms
- Diarrhoea
- Constipation
- Bloody stool (either bright red or very dark)
- Pain in the rectum
- Abdominal pain or discomfort
- More frequent gas, pains or stomach cramps
- Bloating, fullness
- Anorexia
- Cachexia
- Fatigue
Stages of colon cancer:
Stage 0 : Very early cancer on the innermost layer of the intestine.
Stage I : Cancer is in the inner layers of the colon.
Stage II : Cancer has spread through the muscle wall of the colon.
Stage III : Cancer has spread to the lymph nodes.
Stage IV : Cancer has spread to other organs outside the colon.
Diagnosis
- Blood Test
- Colonoscopy with Biopsy
- CT Scan
- PET Scan
- Procto sigmoidoscopy
Treatment
- Surgery
- Chemotherapy
- Radiation Therapy
- Targeted therapy
Complications
- Bowel obstruction
- Cancer returning in the colon
- Metastasis
- Development of a second primary colorectal cancer
Cancer of Anus
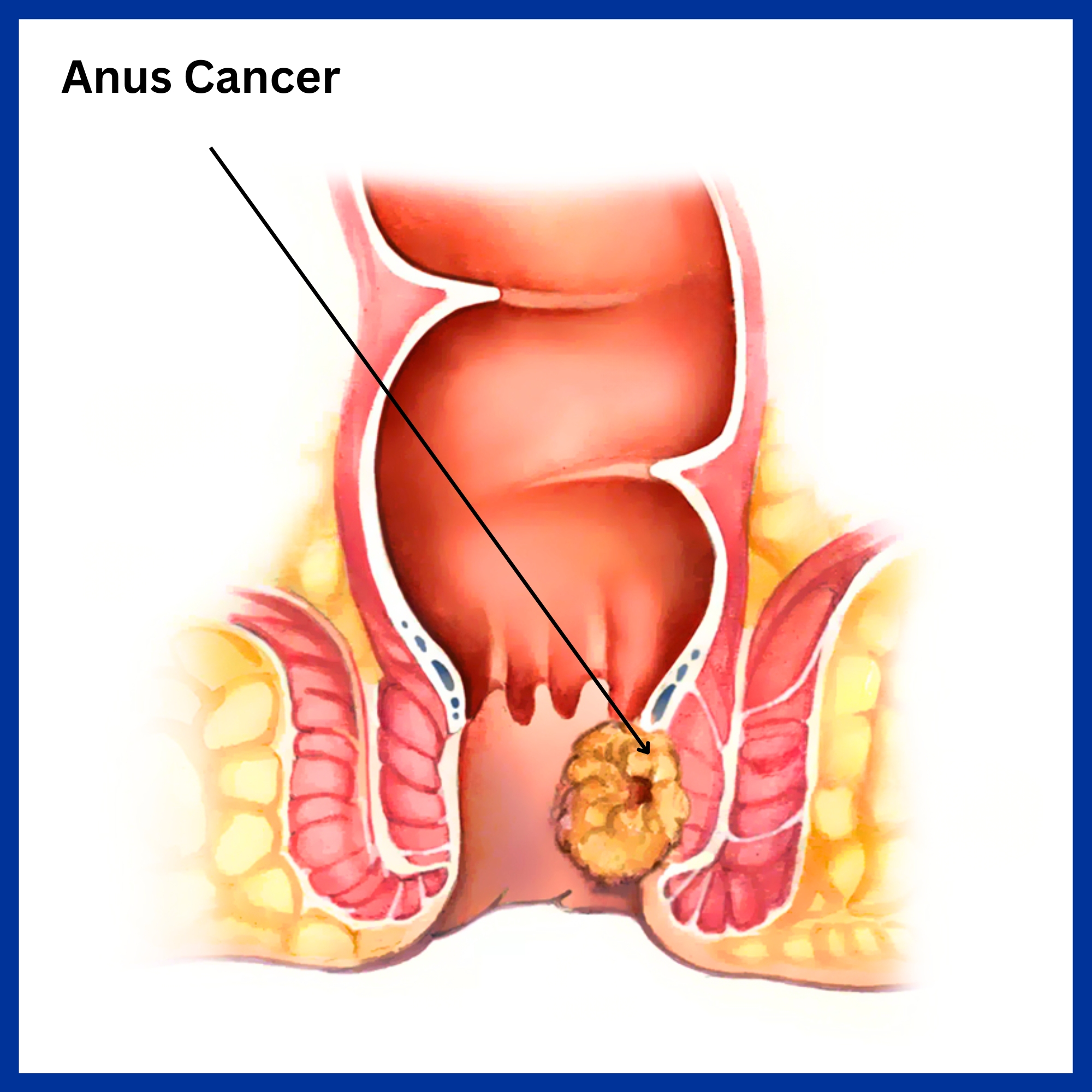
pain or pressure in the anus or rectum, a change in bowel habits, a lump near the anus, rectal bleeding, itching or discharge. Bleeding may be severe
Risk factors
- Human papillomavirus
- Multiple sexual partners
- Smoking
- Immunosuppression
- Benign anal lesions
Symptoms
- Perianal pain
- Perianal itching
- Unusual discharges from the anus
- Change in bowel habits
- Lump near the anus
Diagnosis
- Digital rectal examination
- Proctoscopy
- Colonoscopy
- EUS with biopsy
- CT Scan
- MRI
- PET Scan
Treatment
- Chemotherapy and Radiation
- Surgery
WHY KAIZEN ?
With a vision to extend World Class healthcare solutions to the community through advances in medical technology, medical research and by adopting best man power management practices , Kaizen hospital was established in Ahmedabad in 2011.
HOSPITAL ADDRESS
132ft. Ring Road, Helmet Circle, Memnagar, Ahmedabad – 380052. Gujarat, India.
EMERGENCY( 24X7 )
Mobile: +91 – 99047 44410
Help Line : +91 – 98244 40044
+91 – 79 – 2791 4444
E-MAIL ADDRESS
contact@kaizenhospital.com

