Duodenum Disease
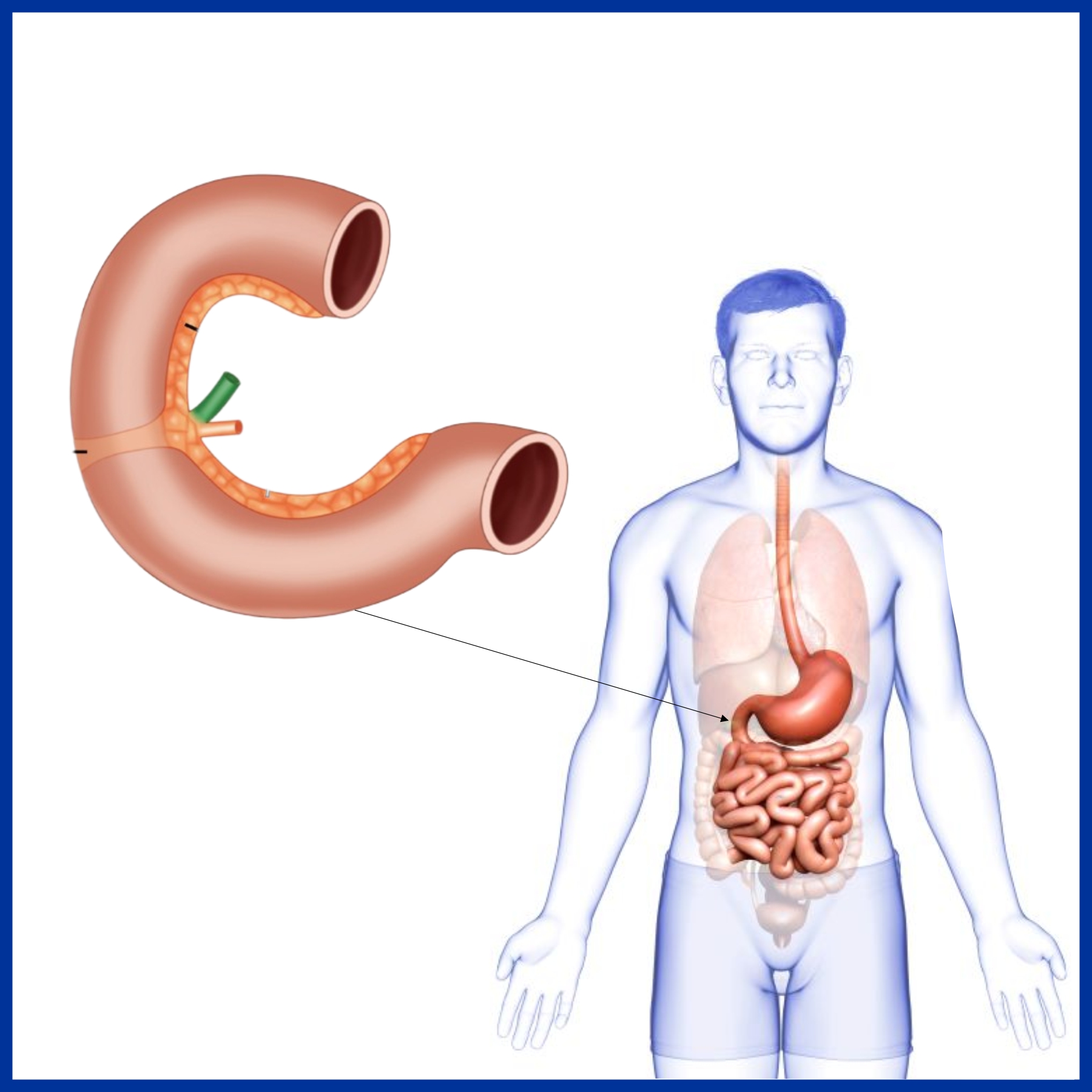
In humans, the duodenum is a hollow jointed tube about 10-15 inches long connecting the stomach to the jejunum. It begins with the duodenal bulb and ends at the suspensory muscle of duodenum. The duodenum precedes the jejunum and ileum and is the shortest part of the small intestine, where most chemical secretion takes place.
Function:- The duodenum is the first and shortest segment of the small intestine. It receives partially digested food (known as chyme) from the stomach and plays a vital role in the chemical digestion of chyme in preparation for absorption in the small intestine.
Duodenal Ulcer
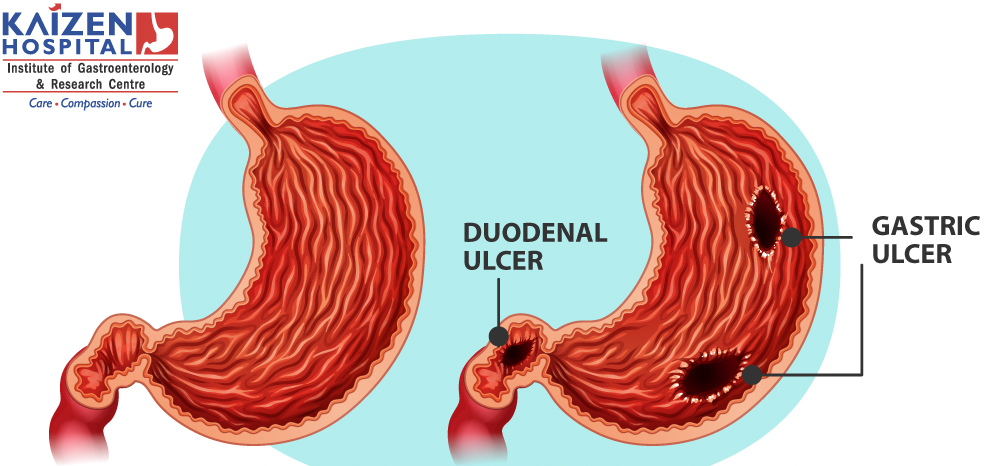
A duodenal ulcer is a type of peptic ulcer that occurs in the duodenum.
- Abdominal bloating, Belching, Feeling of fullness
- Nausea, vomiting
- Unexplained weight loss
- Anorexia
- Burning in stomach
- Upper abdominal pain
- Bloody, tarry stool
- Haemetemesis
- H Pylori Bacteria
- Alcohol
- Tobacco
- NSAIDs
- Radiation Therapy
- Stress, severe illness
- Lifestyle changes such as avoiding oily, spicy foods. Avoid smoking, alcohol and NSAIDS.
Antibiotics
- Proton Pump inhibitors
- Histamine H2-receptor antagonists
Complications
- Perforated duodenal ulcer, which can lead to bleeding
- Internal haemorrhage
- Spread of infection
- Cancer of duodenum
SMA Syndrome

Sign and Symptoms of SMA Syndrome
- Severe postprandial epigastric pain
- Nausea, vomiting
- Early satiety
- Eructations
- Abdominal distention with tenderness
- Diarrhoea
- Subacute small intestinal obstruction
- Symptoms relieved in the left lateral or knee-to-chest position, or in the prone position. Symptoms can be aggravated in right orsupine(face up) position.
- Succussion splash on abdominal examination
Cases of SMA Syndrome
- Aesthenic (thin) body built
- Visceroptosis
- Lax abdominal wall
- Lumbar lordosis, scoliosis
- Anorexia Nervosa
- Cachexia
- Abdominal trauma
- Burns
- Retroperitoneal tumours
- Cancer
- Starvation
- Malabsorption
- Prolonged supine bed rest
- Spinal cord injury
- Scoliosis surgery
- Left nephrectomy, ileo-anal pouch surgery
- Dietary disorders
- Anatomic anomalies- High and fixed position of the ligament of Treitz with an upward displacement of the duodenum, intestinal malrotationaround an axis formed by the SMA.
- Unusually low origin of SMA.
- Familial superior mesenteric artery syndrome
- Traumatic aneurysm of the superior mesenteric artery after a stab wound
- Recurrent superior mesenteric artery syndrome
- Abdominal aortic aneurysms and mycotic aortic aneurysms
- Upper GI scopy
- Colonoscopy
- X Ray Abdomen
- USG Abdomen
- CT Scan
- CT Angiography
- Upper GI series
- Hypotonic Duodenography
- Resolution of underlying conditions, reversal or removal of precipitating factor and weight gain.
- Adequate nutrition, fluids and electrolytes replacement either by inserting jejunal feeding tube, nasogastric intubation or peripherally inserting central catheter (PICC line) administering total parenteral nutrition (TPN).
- Proper positioning of the patient after eating (ie, left lateral decubitus, prone, knee-to-chest position).
- Daily monitoring of patient’s weight.
- Orally liquids can be started followed by slow and gradual introduction of small and frequent soft meals as per patient’s tolerance.
- Prokinetic agents such as Metoclopramide.
- Surgery- Duodenojejunostomy or Gastrojejunostomy.
Complications
- Dehydration
- Electrolyte imbalance (eg, hypokalemia, hypochloremia, metabolic alkalosis)
- Oliguria
- Hypotension
- Malnutrition
- Aspiration pneumonia
- Peptic ulcer disease
Duodenal Perforation
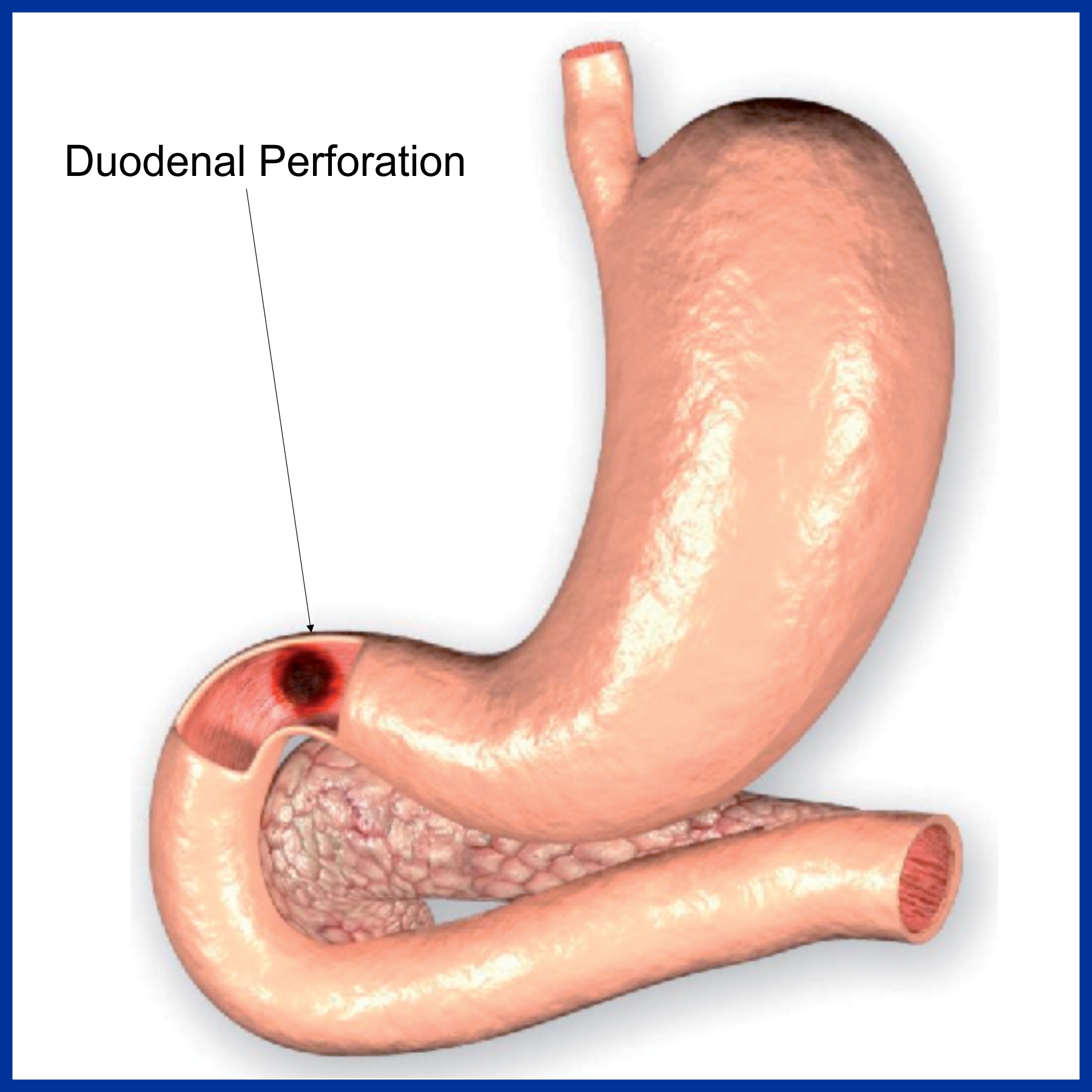
Duodenal perforation is an uncommon complication of endoscopic retrograde cholangio-pancreatography (ERCP) and a rare complication of upper gastrointestinal endoscopy.
Causes of Duodenal perforation
- Blunt abdominal trauma.
- Penetrating injury to the lower chest or abdomen (e.g. stab injuries).
Bacterial infections of Duodenal perforation
- Ingestion of aspirin, non steroidal anti-inflammatory drugs (NSAIDs), and steroids.
- Inflammatory bowel disease (IBD).
- Predisposing conditions – Peptic ulcer disease, acute appendicitis, acute diverticulitis, and inflammed Meckel diverticulum.
- Endoscopy related bowel injuries- Endoscopic biliary stenting, Colonoscopy, ERCP.
- Laparoscopic intestinal injury.
- Bowel perforation by intra-abdominal malignancy, lymphoma, or metastatic renal carcinoma – Even benign tumours, such as desmoid tumours.
- Radiotherapy of cervical carcinoma and other intra – abdominal malignancies.
- Perforation secondary to intestinal ischemia (e.g. ischaemic colitis)
- Necrotizing vasculitis.
- Kidney transplantation
- Foreign bodies (e.g. toothpicks).
- Ingestion of caustic substances – Accidental or suicidal ingestion.
Signs and Symptoms of Duodenal perforation
- Abdominal pain- Sharp, severe, sudden in onset.
- Vomiting
- Hiccoughs
- Board-like rigidity of abdomen with tenderness
- Tachycardia
- Fever
- Absence of bowel sounds
Diagnosis of Duodenal perforation
- CBC
- LFT
- RFT
- Blood culture
- X Ray Abdomen Erect
- Chest PA
- USG Abdomen
- CT Scan
- Laparoscopy
Treatment of Duodenal perforation
- Intravenous access, and crystalloid therapy in patients with clinical signs of dehydration or septicaemia.
- Do not give anything by mouth.
- Intravenous administration of antibiotics.
- Surgery
Complications
- Localized abdominal abscess
- Wound infection
- Mechanical intestinal obstruction
- Postoperative delirium
- Multi organ failure
- Gastrointestinal mucosal hemorrhage
- Fluid and electrolyte imbalance
- Renal failure
- Septic shock
Cancer of Duodenum
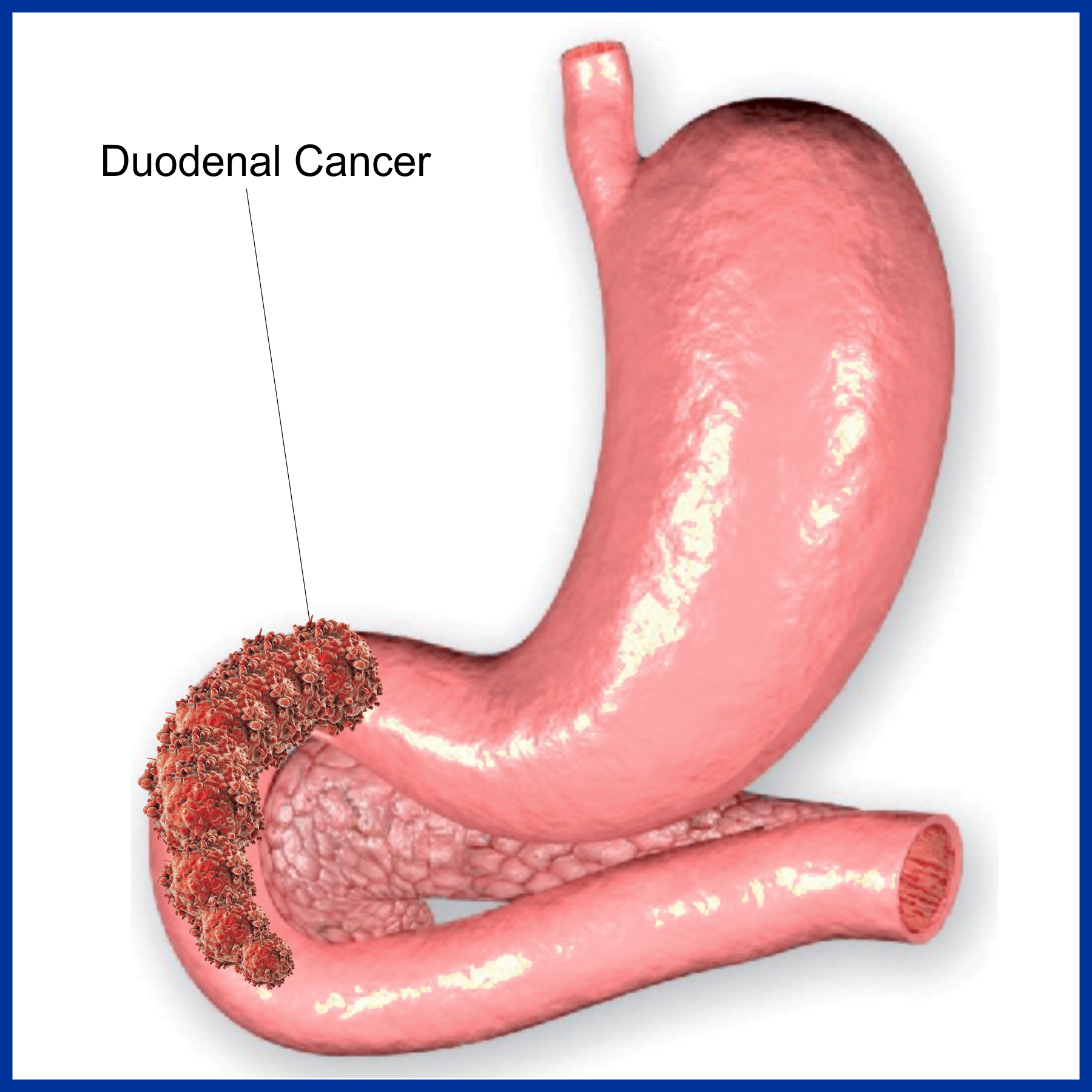
Duodenal cancer is a cancer of first part of the intestine called duodenum, which is a vital organ of digestive tract where bile juice, pancreatic juice and gastric juice are mixed and act on food material.
Risk Factors of Duodenal cancer
- High Fat Diet
- Crohn’s disease
- Celiac disease
- Duodenal ulcer
- Juvenile polyposis syndrome
- Familial adenomatous polyposis (FAP)
- Muir -Torre syndrome- inherited disease caused due to genetic defect.
- Peutz-Jeghers syndrome – Inherited autoimmune disease.
- Heart burn, regurgitation
- Nausea, vomiting
- Bloating
- Weight loss
- Fatigue, generalised weakness
- Abdominal pain
- Melaena
Investigations of Duodenal cancer
- CT Scan
- X Ray Abdomen
- UGI Endoscopy with biopsy
Treatment of Duodenal cancer in india
- Treatment depends on patient’s age, health status and cancer stage.
- Surgery
- Chemotherapy
If you’re specifically Searching for the best gastroenterologist near me, Kaizen Hospital boasts a team of highly skilled and experienced gastroenterologist doctors dedicated to providing exceptional care
HOSPITAL ADDRESS
132ft. Ring Road, Helmet Circle, Memnagar, Ahmedabad – 380052. Gujarat, India.
EMERGENCY( 24X7 )
Mobile: +91 – 99047 44410
Help Line : +91 – 98244 40044
+91 – 79 – 2791 4444
E-MAIL ADDRESS
contact@kaizenhospital.com
WHY KAIZEN ?
With a vision to extend World Class healthcare solutions to the community through advances in medical technology, medical research and by adopting best man power management practices , Kaizen hospital was established in Ahmedabad in 2011.

